- Home
- Injections
- Laser Treatments
- Specialties
Specialtiesview all
- Other Treatments
- Before After Photos
Before After Photosview all
- Contact Us
- Doctor And Staff
- About Celibre
- Blogs
Syringoma are small, non-cancerous growths that most commonly show up on your lower eyelids and upper cheeks. They are more common in women than men, and we see them more often in Asian women than any other patients. While they’re not dangerous, they can be cosmetically undesirable. You might think that removing these on the delicate eyelid skin would be impossible, but it isn’t! We’ve performed successful syringoma removal for many patients, so don’t let you fear hold you back from seeking treatment.
Many of our patients think that we’ll need to use an aggressive treatment, like a fractional laser. We like to think of this as using a sledgehammer to pound in a nail—it’s overkill. Sure, we could use a form of laser resurfacing, but syringoma are so small that the trouble we’d go through just wouldn’t be worth all the fuss.

Here are some before and after photos of one of our patients in the Los Angeles area who was treated with hyfrecation.
There is another treatment that is much easier but works just as well: hyfrecation. Hyfrecation involves using a thin, needle-like probe that is attached to an adjustable electric current. This tiny probe can be used very precisely to target the individual syringoma. The electrical current heats the tissue which destroys the bumps. It’s a fast, simple procedure that works very well.
If you have syringoma and are ready to get rid of them, give us a call today.
The short answer to this common question is no. Unfortunately, we still don’t have a cure for Rosacea. And we really don’t have a solid understanding of what exactly causes it either. The factors causing Rosacea are varied and they often can be different for different patients. This also makes finding one, single treatment that is effective for everyone a challenge as well. If you struggle with Rosacea but haven’t tried laser treatments, perhaps it’s time.
Many patients like you suffering with Rosacea come to us because they have failed medication options. We often find that many patients don’t understand the nature of their condition and that it isn’t curable. They often don’t know that Rosacea is a triggered process, meaning that there are things that can be done to avoid a flare.


Rosacea before and after photos
During consultation and treatment, we help patients like you suffering with Rosacea to better understand and manage the condition. While Rosacea may not curable, it’s certainly manageable. We use safe, proven light-based and laser treatments such as pulsed dye lasers and PDT, or photodynamic therapy, to reduce the redness and excessive blood vessels triggered by Rosacea. These treatments offer dramatic improvement—usually much more than with prescription oral and topical medications.
When you visit, we take the time to discuss your Rosacea with you and help you identify possible triggers such as spicy foods, alcohol, heat or coffee in addition to offering an effective laser treatment option. While we know there’s no cure Rosacea, and we’ve helped thousands of patients like you in the Los Angeles and torrance area take control of and improve on this frustrating skin condition.
If you keep up with the latest news in laser tattoo removal, then you know that the PicoSure laser is the “latest and greatest” to hit the scene. What’s different about it is that it delivers a burst of light in a slightly faster pulse than other tattoo removal lasers—a picosecond rather than a nanosecond. What makes it better? Well, the theory is that this increased speed breaks up the ink particles into smaller “bits” that the body can then clear away more quickly and in larger numbers per treatment compared to nanosecond devices. This means faster clearance of a tattoo and total clearance in fewer treatments.
When patients come in asking about the PicoSure, we explain this to them, but what the direct-to-consumer marketing doesn’t inform them about is the type of light this laser uses. It is a 755 nm wavelength, which isn’t the same as most other lasers used for tattoo removal. The Nd:Yag is the most common, which utilizes a 1064/532 nm wavelength. Remember, tattoos consist of colored ink particles embedded within the skin, and the most common color used is black. The optimal color absorbed by a 755 nm wavelength is green.
Here is an excerpt from Wikipedia that may help you better understand how the q-switched 755 nm (Alexandrite) laser works and the reasons why it’s not the best for most dark-colored tattoos:
“Q-switched Alexandrite: 755 nm. The weakest of all the q-switched devices and somewhat similar to the Ruby laser in that the Alexandrite creates a red light which is highly absorbed by green and dark tattoo pigments. However, the alexandrite laser color is slightly less absorbed by melanin, so this laser has a slightly lower incidence of unwanted pigmentary changes than a ruby laser. This laser works well on green tattoos but because of its weaker peak power it works only moderately well on black and blue ink. It does not work at all (or very minimally) on red, orange, yellow, brown, etc. This laser wavelength is also available in a picosecond speed with anecdotal claims that it removes ink faster.” **
** Reference http://en.wikipedia.org/wiki/Tattoo_removal.
We understand that if you have an unwanted tattoo, you want to find the fastest, most effective, safe and cost-effective way to get rid of it. But, laser medicine is a highly technical and complex field that not everyone (even some practitioners) can understand. Just like tattoo artists, there are different levels of skill and knowledge when it comes to laser tattoo removal practitioners. Finding one that has the proper expertise, skill and knowledge of laser physics along with the right laser for your tattoo color is your best bet to get the best outcome. The PicoSure laser might be the right choice of laser for you, but it might not be. It depends on the colors you have in your tattoo.
Be responsible and do your homework. Don’t fall for advertising, flashy marketing or other gimmicks. Research which lasers use wavelengths that are appropriate for the colors in your tattoo and then find a good laser practitioner with lots of experience using that device and treating other patients of your skin type (color). We promise you that this is the best way to get the results you’re looking for!

Are you dealing with Melasma, the difficult and frustrating condition often referred to as the pregnancy mask? Or are you struggling with brown scars from acne breakouts? Having clear, healthy-looking skin is what most of us want, regardless of the condition we are struggling with.
At Celibre Medical, we’re experts at dealing with difficult pigmentation problems like Melasma and acne scars. Many patients who’ve come to us struggling with Melasma or hyperpigmentation have tried (and failed) several different products or treatments.
One of the most common is TriLuma. It is a prescription cream that is very common in our industry and has 4% hydroquine as well as Retin A to exfoliate the skin and a steroid to combat irritation. Its formulation is based on the premise that inflammation is part of the process that stimulates pigmentation (in melasma and acne, etc.).


Melasma before and after pictures
Cosmelan MD is a bit different. Cosmelan MD is a very aggressive Retin A and hydroquinone based peel that usually involves 3-4 days of recovery time. And that’s the main complaint among patients. They don’t want to take time off of work. Although we have found Cosmelan to be useful in situations where a patient has very little time to prepare for a big event (wedding, birthday, etc.), it is also a very expensive product, with the peel and take home product often running at $600 or more (2018) and it has 3-4 days of recovery.
Over the past 15 years, we’ve used both Cosmelan and Triluma for our patients. Triluma is a bit more expensive than we would like, but there are three issues that prevent us from recommending it. First is the ongoing use of a steroid, which can thin the skin. Second is the 4% hydroquinone, it’s not enough for many patients. Finally, the cream formulation is good for shelf life, but not for deep penetration. We prefer a gel based solution for better penetration.
We’ve settled on the Celibre Medical depigmentation program for several reasons. First it’s affordable. Celibre Medical depigmentation pads are significantly less than Triluma and about 20% of the cost of Cosmelan. We want patients to have convenience when managing their Melasma. Celibre Medical depigmentation pads can be used at home, do not require any downtime and can be shipped directly to your address. This is convenience at its best. Finally, and most importantly, we want the product to work well. Our 8% gel based pads work better than any other Melasma product we have used over the past 15 years. The higher strength hydroquinone combined with the increased absorption associated with the gel formulation mean better results for you.
While there’s no one regimen that works for everyone, we believe the Celibre Medical depigmentation program is superior to Triluma and Cosmelan MD because of the superior results, ease of use and affordable cost.
Hydroquinone is a lightening or bleaching medication that has been added to over-the-counter and prescription products for many years. It offers the ability to “bleach” and even out skin tone. Most people who use hydroquinone-containing products want to treat skin problems that cause brown spots such as melasma, sun damage, freckles, or scars. Hydroquinone works by slowing down the skin’s production of melanin (or pigment), so it won’t change the underlying color of your skin, but will help overly pigmented areas fade to your normal skin tone.

At Celibre Medical, we often see the following scenario in patients with darker or ethnic skin. Many hydroquinone creams are used with or even combined with retinoids (Retin-A) into a single product. These two compounds together can cause irritation. Ethnic skin, when inflamed and irritated, frequently responds by making more pigmentation. Although their skin feels irritated, many patients see this increased discoloration and use even more of the cream to fight it! This leads to a vicious cycle of irritation, inflammation and a worsening of a pigmentation problem. This unfortunate cycle could have simply been avoided by some up-front education on how hydroquinone works and its typical effects on the skin. The way to avoid this problem is to use the product conservatively without leaving dabs on the skin for long periods.
A more serious potential concern with the use of hydroquinone on darker, ethnic skin is the problem of ochronosis. In this condition, hydroquinone-containing creams (usually higher strength, 8% to 10% prescriptions) trigger the gradual development of a blueish-grey discoloration in the skin. This side effect can be avoided by using no higher than 8% hydroquinone, taking breaks from the medication use every three months and avoiding sun exposure when using the medication.
If you are considering using hydroquinone, take the time to speak with your medical practitioner and discuss all the possible effects (good and bad) of hydroquinone before you use it. Hydroquinone is a powerful medication that has the potential to do good, but can cause problems if not used correctly or without proper follow up care.
It’s important to remember that hydroquinone may not be the best choice for your pigmentation problem. Class IV medical lasers also offer an effective treatment option (especially for sun damage) if you’ve failed hydroquinone or are not a good candidate for it.
Lori Ishii Haney, RN, MEP-C
Certified Medical Laser Safety Officer
Before you think having an accessory (extra) nipple sounds weird or crazy, keep in mind that it’s relatively common: about 1 in every 20 people has one! Accessory nipples can occur in both men and women and are not a sign of an underlying medical problem or genetic defect. Sometimes, in mammals (including humans) this excess tissue forms in the same vertical (up and down) plane just below the real nipple on the chest or abdomen.

Many people don’t even realize that they have one of these because the “extra” nipple is not as developed as your real ones. You may simply mistake it for a mole or skin tag. So, what do you do if you have one? Usually nothing! They are really a cosmetic concern, and there’s not a medical reason to remove them. Still, many people with accessory nipples want to have them removed.
The best treatment is surgical excision by either a qualified general surgeon or a plastic surgeon. The reason that the nipple requires surgery is that it may reoccur if all the tissue is not completely removed. If you decide to pursue surgical excision and wind up with a scar from your procedure, we can help you with class IV medical lasers. These devices are excellent for reducing excessive color and improving the texture of scar tissue.
When you think of sunscreen, what do you think of ? Sticky, greasy and uncomfortable, but a necessary evil? Do you think about skin cancer or sunburn prevention? Do you think about the beach, pool or vacation? If so, you’re like most of us. We often think about sunscreen for “special occasions” where we have extended exposure to the sun. But do you realize that every day, even if you work indoors. You are exposing your skin to harmful UV rays that can damage and age it? Although you may not have thought of sunscreen as a daily necessity to slow the aging process—but we think you should!
Photoaging is the term that we use for this slow, long-term type of sun damage that occurs over many years without sunscreen. It can make your skin look rough with an uneven texture, discolored and even contribute to loose or saggy skin. Of course, it’s the major contributor to the development of fine lines and wrinkling as well.


Photoaging resulting from lack of sunscreen use
Yes, skin cancer is worrisome and should be motivation for you to use sunscreen. Even a very slow accumulation of UV damage over an extended period can cause precancerous changes and skin cancer! The bottom line is that Southern California residents should wear a good, broad-spectrum sunscreen every day to protect their skin.
If you’re thinking it’s too confusing to pick out one that you like and would be willing to wear every day—you might be right! It can be harder than you think to find one that checks all the safety boxes and also feels nice enough to put on every day. The FDA has tried to make the process a bit less confusing by requiring sunscreen manufacturers to be clearer in their labeling of SPF or “sunburn protection factor”. They have also made a public education push to help consumers understand that a higher SPF doesn’t mean a “better” sunscreen. In fact, a product with an SPF of 100 provides no better protection from harmful UV radiation than one with an SPF of 50.
So, now that you know that you don’t need a higher SPF than 50, what else should you know? Surprisingly, a lot! How and when you use your sunscreen matters, so we’ve comprised a tip list here on this page to help you get the most out of your sunscreen! Here it is:
Don’t take your chances! Now that you know more about sunscreen, pick a good one and use it correctly every day to keep your skin looking young and healthy.
Have you used a bleaching cream in the past for your melasma and had to stop because it made your skin red, dry and irritated? If you answered yes, you’re not alone. We’ve had many melasma patients come to us afraid to use hydroquinone for their Melasma because of a negative experience like this. We spend a lot of time with these patients educating them on the importance of finding the right formulation and understanding how this important medication works to help control their frustrating Melasma.
It’s important to understand that it’s usually not the hydroquinone that causes the irritation. Most formulations designed to treat melasma also contain tretinoin (Retin A) and a steroid. It’s usually the Retin A that is the troublemaker. The steroid is added to help counteract the irritation of the Retin A, but it’s often not enough to avoid it altogether.
So why is Retin A added to bleaching cream? Because for those who can tolerate it, it works well to enhance and speed the effect of the hydroquinone. Retin A stimulates skin cell turnover or exfoliation. When you combine this with the pigment reducing effect of the hydroquinone, it can help your skin look clearer faster. But most people find it too irritating—even at lower concentrations and with the addition of a steroid. Bottom line is that if you can’t use it, then it’s not going to work!
We realized some time ago that Melasma patients need effective yet gentle formulations of hydroquinone. Here at Celibre, we’ve designed hydroquinone pads that use a hydroquinone gel in strengths of 4%, 6% or 8% WITHOUT Retin A. These formulations are more tolerable for most patients and they allow us to customize the strength of your treatment depending on your specific needs. If you need a progressive approach, we can go slow and allow you to build tolerance over time.
Our program is unique in that we have options. We’ve helped many Melasma patients improve after failing a more traditional treatment approach. If you’re looking for a personalized, tailored treatment plan for your Melasma, then come see us today. We would love the opportunity to discuss how our customized approach can help meet your goals.

Photodynamic Therapy (or PDT) is a great treatment for anyone who has sun damage, precancerous spots, acne and/or rosacea. It involves the use of both light and a medication that makes your skin sensitive to the light. As well as it works to improve and/or correct these underlying skin conditions, it is considered an aggressive treatment. If you’re considering having PDT, there are a few things that you need to think about before your treatment. At Celibre, our PDT consultations include a discussion about each of the following:
When all things are considered, we believe that the potential benefits of having PDT far outweigh the risks of any of these unwanted side effects. Still, it is our job to educate and inform you of them so that you can truly make the decision for yourself.


Do you have one or more tiny, raised bumps around your eyes or on your lower eyelids? If so, you may have syringoma, a fairly common condition that usually affects women. The bumps are pinpoint in size, usually between 1 and 3 millimeters. They are white, flesh-colored or yellow in appearance.
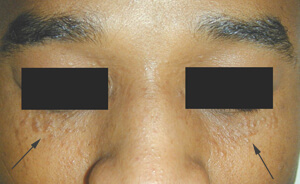
If you’re worried that they are a health risk, you can relax. Syringoma are harmless, but are aggravating to patients like you because they change the texture of your skin. If you have them and want to get rid of them, we’ve got an option.
The two best ways to treat syringoma are with electrodessication and ablative laser treatments. Both these methods destroy the excess tissue that make up the syringoma. As you might imagine, treatment can be tricky since syringoma are small in size and close to your eyes, so pick a practitioner with the right equipment and experience.
Electrodessication uses a very fine needle that is inserted on top of the growth. It passes an electric current into the tissue, heating it up and shrinking it which makes it go away as it heals. Ablative laser therapy may involve an erbium or CO2 laser to vaporize the excess tissue! We typically refer electrodessication as the hyfrecator allows us to be very precise with the placement of heat energy.
If you have Syringoma and would like to learn more about treatment, call us today.
Do you have a darker skin type and wish that you could have laser resurfacing? Well, guess what? You can! But you’re not a candidate for every type of procedure, and you need to make sure that you partner with an experienced laser practitioner who has access to the specific type of device that is right for you.

Here at Celibre Medical, we offer personalized, expert care that includes laser resurfacing for darker skin types such as those who are of Asian, Hispanic or African American decent. We have heard over and over from these patients how they’ve previously been told that laser resurfacing wasn’t an option for them. This just is untrue. However, to get the results you are looking for and avoid unwanted complications, the correct technology must be used. We have more than 10 different devices in each of our Los Angeles and Torrance offices that can get the job done, and we use the Sciton Profractional laser (Erbium) to avoid side effects with darker skin types.
Below are photos of one of our patients who underwent fractional laser resurfacing of a traumatic forehead scar. She was thrilled with her results and you will be too! Please give us a call today to learn more about our fractional laser resurfacing program today.
Even we admit, it can be hard to tell these two apart sometimes! But they are different and usually require different forms of treatment to clear them up. This is why self-diagnosis or self-treatment can be risky. If you treat one as the other or vice versa, you can make things worse.

Let’s start with milia. These are small, pinpoint white bumps that usually pop up on the oily areas of the face. They will come and stay, and sometimes, you feel them more than see them. They happen when dead skin cells become trapped beneath a few cell layers of the skin. In essence, they are very small cysts and completely harmless. Pretty much anyone can get them—and up to 50% of newborns have milia! They are also common in kids, teens and adults. If you have an oilier skin type, then you may be more prone to developing milia, but it’s important to note that it is not a form of acne or related to acne.
Treatment revolves around a couple different things. Number one, you should control your oil. This is easily done with skin care products that contain either glycolic acid or retinols. This will help you prevent milia. But what about the milia that are already there? The most common way to get rid of them is to “extract” them. This involves opening the milia and getting the clump of dead skin cells out. While it seems straight forward, it can be tricky and we’ve seen several instances where extractions done by both patients and aestheticians resulted in icepick type acne scars because they were too aggressive. An alternative treatment is the use of q-switched lasers combined with topical products to remove milia. This is generally very safe and results in good clearance.

Now, onto acne. There are few different forms of acne and most people who suffer with it have a mix of these forms: comedones, papules and/or nodules and cysts. It is the comedonal form of acne that is most often confused with milia. Specifically, closed comedones. What’s the difference? A closed comedone is often referred to as a “whitehead” because it is a plugged oil gland that is not inflamed, but is covered by a thin layer of skin cells that protects it from contact with the air. The other is an open comedone or a “blackhead”. It is the exactly the same as an open comedone, but the difference is that there is no covering so it is exposed to contact with the air. This changes the sebum (oil) that’s in the plug and makes it turn dark or “black”.
Treatment of comedonal acne is first and foremost dependent on a strict regimen of good skin care. Again, glycolic acid containing products or retinols work well to control the oil, and they also help gently exfoliate to dislodge the plugs in the oil glands. If used daily, this often clears up most open and closed comedones. A good jump start or a more intensive treatment can also include chemical peels to further encourage exfoliation. It is important to NOT extract comedonal acne lesions as this can lead to scarring and aggravation of inflammatory acne.
Another alternative treatment is laser therapy for acne. Light based treatments can help curb bacterial growth that is associated with acne. There are also treatments designed with light and light sensitizing medication that can help dry up oil to improve stubborn, resistant acne.
As you can see, it’s important to distinguish which of these two, often confused conditions you have, because treatments vary. The key to any successful treatment plan is correctly identifying what it is that your treating in the first place!
If you’re struggling with acne and have tried and failed numerous options, we understand. Acne is so much more than a skin problem. It can affect every single aspect of your life inside and out. Before you give up, please read this page. We want you to know that there are other options. One acne treatment option that is rarely discussed is photodynamic therapy (PDT).
PDT is a treatment for acne that involves using a medication and a light-based together to reduce inflammatory acne. It works by targeting overactive oil glands. Patients with acne tend to make too much oil, a significant underlying factor for the acne condition.
The medicine used in PDT is called aminolevulinic acid (ALA). When ALA is applied to the skin, it gets absorbed into the oil gland. This process takes from 3 – 8 hours. ALA reacts very strongly to certain types of light. This property is called “photosensitivity”. During PDT, a Blue light is used. This light has a type of light that activates the ALA, thereby decreasing oil production. After 20-30 minutes of blue light exposure, you will look and feel like you have a sunburn. Even patients with darker skin who have never burned in the sun get this reaction.
For most patients with moderate acne, a series of 1 to 3 PDT treatments will improve their acne. Because of the underlying effect on the oil glands, oily skin, flare-ups and active pimples decrease. As you can see by the before and after photos, the results can be dramatic.
If you live in the Los Angeles or Torrance areas and are looking for an alternative treatment to Accutane for your acne, we encourage you to call us and schedule a free consultation to learn more about how PDT can help.


A port wine stain is a type of birthmark. Rather than brown, it’s red and comprised of a network of very tiny blood vessels.
Most port wine stains develop on the face and neck, however, they can occur anywhere on the body. If you have a port wine stain and have considered removing it, laser treatment with pulsed dye lasers works very well.
Port wine stains can be large and deep red or purple in color (hence, the name), so they don’t cover easily with makeup. Pulsed dye laser treatment is perfect for these birthmarks because the light it emits is absorbed by the small blood vessels that make up the birthmark..
Treatment can take time and progress may seem slow at first, but pulsed dye laser treatment has been proven both safe and effective. If you’re ready to have your port wine stain treated, call us today to learn more!

If you’re researching laser treatments for Rosacea, you may have come across the term “bruising treatment” and wondered what exactly it means. Bruising treatment refers to an aggressive type of pulsed dye laser treatment. We offer them here at Celibre Medical, and we answer this question all the time for patients like you.
Rosacea is a condition that involves excessive blood vessels at the surface of the skin. Just like other vascular conditions (spider veins, red stretch marks, acne scars, etc.), the pulsed dye laser works by closing the blood vessels and making them disappear over time.
Bruising treatments are more aggressive, and they are not appropriate for every skin type (color). They also may not be appropriate if you need to get back to work or school immediately. This type of treatment will require you to take a bit of “social downtime”.
Research has shown that bruising treatments can give you the most dramatic results in the shortest amount of time when used to treat Rosacea. So, if they’re right for you, they are a great choice. If not, we still find that our Rosacea patients do very well with non-bruising pulsed dye laser treatments too.

