Fungal acne, which is a very common but misunderstood condition, is normally confused with normal acne. Since it resembles traditional acne, including infections triggered by bacteria, there is a high likelihood of patients administering the wrong products, thus making the breakout experience a series of ongoing problems. Knowing the causes of fungal acne is important in identifying and finding a cure.
Fungal Acne primarily targets individuals who are prone to sweating or stay in a humid environment. Most individuals who are prone to excessive sweating or live in a humid environment are likely to develop Fungal Acne. Having understood what causes this type of Acne, one can clearly see that controlling and preventing Acne
What Is Fungal Acne?
A condition known as fungal acne or Malassezia folliculitis is caused by too much yeast growing on your skin. The Malassezia yeast lives on human skin but can multiply too much on your skin to cause your hair follicles on your skin to get infected.
Fungal acne, unlike bacterial acne, does not involve clogged pores or, in other words, acne-causing bacteria, which is the reason why most standard acne treatment options have failed to provide a solution and in fact cause further problems.

What Causes Fungal Acne?
Fungal Acne results from an environment in skin that is conducive for the multiplication of yeast in the skin.
There are various factors involved in Fungal Acne in both men and women.
Overgrowth of Malassezia Yeast
Every individual carries Malassezia yeast on the skin; but if it grows uncontrollably, it causes infection and leads to smaller bumps as a result of hair follicle inflammations. The environment becomes ripe for yeast overgrowth due to the excess oil, heat, and humidity.
Excess Sweat and Humidity
Sweat and humid environments also raise the risk of fungal acne occurrence greatly. The increase in sweat on the skin causes temperatures to rise, thus creating a perfect environment where yeast can be produced, and this is the reason why fungal acne can also be common during the summer or even in a tropical environment.
Wearing Tight or Non-Breathable Clothing
Tight clothing and synthetic fabrics trap sweat and heat against the skin. This lack of airflow prevents moisture from evaporating, allowing yeast to thrive. Areas covered by tight workout gear or uniforms are especially vulnerable.
Using Pore-Clogging or Oil-Heavy Skincare Products
Many skincare products contain oils, fatty acids, and esters that feed Malassezia. Even products marketed as acne-safe can trigger fungal acne if they include yeast-feeding ingredients. Heavy moisturizers and sunscreens are common culprits.
Antibiotic Use
Antibiotics disrupt the skin’s natural microbiome by eliminating beneficial bacteria that keep yeast in balance. When this balance is disturbed, yeast can multiply rapidly, leading to fungal acne flare-ups, particularly after prolonged antibiotic use.
Weakened Immune System
A weakened immune system makes it harder for the body to control yeast growth. Stress, illness, poor sleep, and certain medications can all reduce immune defenses, increasing susceptibility to fungal acne.
Poor Hygiene After Sweating
Leaving sweat on the skin for extended periods encourages yeast growth. Rewearing sweaty clothes, using damp towels, or delaying showers after workouts can all worsen fungal acne, even in individuals with otherwise good hygiene habits.
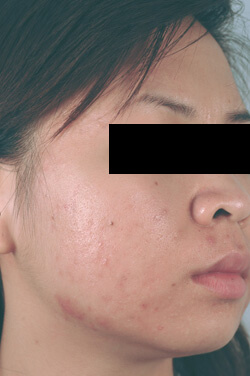
Common Areas Where Fungal Acne Appears
Fungal acne typically develops in areas that produce more sweat and oil. Common locations include the face—particularly the forehead, temples, and hairline—as well as the chest, back, shoulders, and upper arms.
Symptoms of Fungal Acne
Fungal acne often appears as small, uniform bumps that cluster together. Itchiness is a key symptom that helps distinguish it from regular acne. The bumps may become red or inflamed and often appear suddenly or spread quickly.
How Fungal Acne Differs From Regular Acne
While fungal acne and bacterial acne can look similar, they behave differently. Fungal acne does not produce blackheads or whiteheads and tends to be itchy rather than painful. It also does not respond to standard acne treatments and may worsen when treated incorrectly.
Who Is Most at Risk for Fungal Acne?
People who sweat frequently, live in humid climates, have oily skin, or use antibiotics are at higher risk for fungal acne. Athletes, gym-goers, and individuals under chronic stress are also more susceptible due to increased sweat and weakened immune responses.
How to Prevent Fungal Acne
Preventing fungal acne involves controlling moisture and avoiding yeast-feeding products. Showering after sweating, wearing breathable fabrics, choosing fungal-acne-safe skincare, and minimizing unnecessary antibiotic use can significantly reduce flare-ups.
When to See a Dermatologist
If fungal acne does not improve with over-the-counter antifungal treatments or continues to spread, consulting a dermatologist is recommended. A professional diagnosis ensures appropriate treatment and helps rule out other skin conditions.
Key Takeaways
Fungal acne is caused by an overgrowth of Malassezia yeast, triggered by factors such as sweat, humidity, tight clothing, oil-heavy skincare, antibiotics, and weakened immunity. Because it mimics traditional acne, it is often misdiagnosed. Understanding its causes is the key to effective treatment and long-term prevention.

