What Causes Skin Tags on the Face: A Clear, Simple Guide
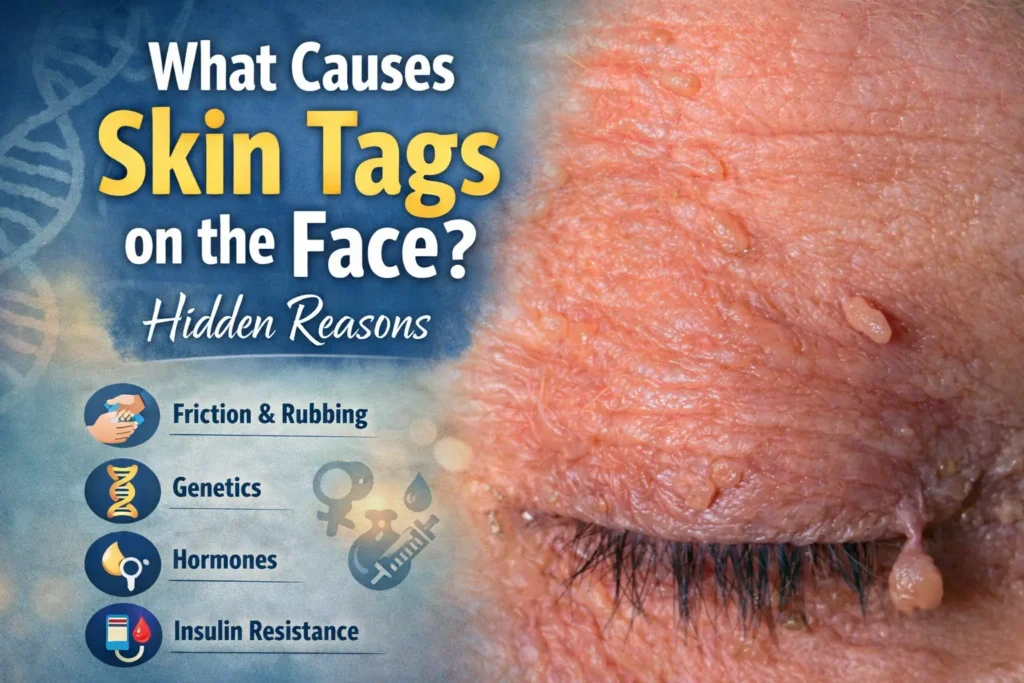
Skin tags are one of the most common benign skin growths, and many people notice them on the face as they get older. They can show up on the eyelids, along the jawline, near the neck or anywhere skin folds or rubs. Even though they’re harmless, most patients are curious to understand why they appear […]
What Causes Cherry Angiomas?

A cherry angioma exists as a tiny red skin lesion which shows up on most adults as part of the aging process. These growths are harmless although their appearance can confuse patients the first time they see them. Most people worry when new red spots appear on the body or face, but cherry angiomas are […]
Will Using Mineral Makeup Help my Acne?

Safe and Tailored Acne Patient Treatment Plans At Celibre Medical, we treat acne differently. We recognize that acne affects far more than just your skin—it can impact your confidence, daily routines, and overall quality of life. That’s why we focus on delivering safe, innovative, and fully personalized acne treatment plans designed around your individual needs. […]
Are We Being Vain with Botox?

It’s not unusual for patients—both men and women—to pause and question their motivations when considering aesthetic treatments. During consultations, these conversations arise more often than one might expect, and they are almost always thoughtful, sincere, and rooted in self-reflection rather than vanity. Men often ask with genuine curiosity, “Do many men get these treatments?” Women, […]
Photodamage and Aging

Photodamage and Skin Aging: How Sun Exposure Accelerates the Aging Process Some things improve with age—fine wine, artisan cheese, and a perfectly worn pair of jeans. Unfortunately, skin is not one of them. If you’ve noticed early signs of aging such as fine lines, wrinkles, or uneven skin tone, you’re not alone. Many people explore […]
How to use sunscreen on Face
By now, most patients understand how important it is to wear sunscreen. However, while many people apply sunscreen regularly, we are often surprised to learn that very few truly understand how to use sunscreen on face and body effectively. We spend time educating our patients on the importance of proper sunscreen use for overall […]
What Do Sun Spots Look Like?

Sun spots are one of the most common changes our patients notice as they get older. Most that get them have spent a lot of time in the sun. Understanding their appearance is valuable because this helps determine the right course of treatment. What are Sun Spots Sun spots, often called solar lentigines, are flat […]
What Does Brow Shaping Mean?

You’re browsing Realself and you keep coming across the term “brow shaping” If you’re thinking this term relates to plucking, tweezing, or waxing the eyebrows, think again! In the aesthetic world, brow shaping refers to techniques and treatments that change the position, lift/arch, and/or volume of the eyebrow and the area around it. Why Brow […]
How Fillers Can Help Hide Dark Circles Under Eye

Under Eye Filler Dark Circles Are dark circles under the eyes making you look tired? Do friends or loved ones ask if you’ve had enough sleep? If you have hollowing, shadowing, puffy eye bags or darkening under the eyes, then you may be a good candidate for an exciting procedure known as tear trough correction. […]
How to Remove Brown Spots on Face?

Brown spots on the face are a common concern that many of our patients notice as they age or spend time in the sun. The skin develops spots with prolonged sun exposure and aging. Many of these spots do not pose a health concern but they may affect how you feel your skin and appearance. […]
How to Get Rid of Dark Spots on Body?

Dark spots on the body are a common concern for many of our patients. The skin develops these spots – hyperpigmentation, sunspots or age spots – over time, and they can be present on any part of the body including arms, legs, back or chest. The spots are often harmless sun damage, but they create […]
What Gets Rid of Acne Scars: Treatments and Products

Acne scars are a concerning after-effect of past acne breakouts. Our patients seek effective products and treatments for improving their acne scars. Acne scars exist in various forms such as surface indentations, pinpoint holes as well as red and brown discoloration. Suitable treatment methods depend on your skin and scar type. Acne Scars Overview Skin […]
What is Rosacea?

Do you notice persistent redness, irritation, flaking, or acne-like bumps on your face that won’t go away even past your mid-twenties? You may be dealing with rosacea. While it’s often recognized by facial redness, this chronic skin condition can also cause discomfort, sensitivity, and breakouts that resemble acne. Unfortunately, rosacea has no known cure. However, […]
Can Teeth Grinding Cause Migraines?
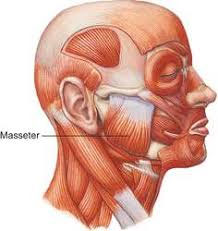
If you’ve ever wondered, “Can teeth grinding cause migraines?”—the answer is yes, it can. Many people don’t realize that chronic jaw tension and clenching, also known as bruxism, can trigger migraines, headaches, and even neck or shoulder pain. When I meet patients seeking injections like Dysport, Botox, or fillers, I always look for signs of […]
What is Melasma?

While it may sound like a fancy, unusual word, melasma is a very common skin condition. You might have noticed dark brown patches on your cheeks, forehead, or upper lip—maybe even thought it was just your skin reacting to the sun. These patches often appear suddenly—during pregnancy, while taking birth control, or even after a […]
